A new study has examined the relationship between socioeconomic status and prescribing magnitude and cost in primary care throughout Northern Ireland.
The study analysed open-source data collected from 325 GP practices in Northern Ireland from May to October 2019, to determine the number of prescriptions, cost of drugs and drug classes by area, ranking these by deprivation index. A total of 2,764,303 prescriptions were signed during the study period.
The analysis indicated a trend of increased overall spending per patient (r=-0.1232; P=.02) and the number of prescriptions per patient (r=−0.3440; P<.001) in areas of higher deprivation.
The mean cost per item was higher in less deprived areas (r=0.3809, p<0.001). Overall, £13.79 more was spent and 3.5 more items were prescribed per patient in the most compared with the least deprived decile. More expensive items tended to be prescribed in areas with lower socioeconomic deprivation (£11.27 per item vs £9.20 per item).
There was a statistically significant correlation of prescribing of key drug classes, such as bronchodilators, antidepressants and drugs used to treat diabetes, among others, with greater deprivation.
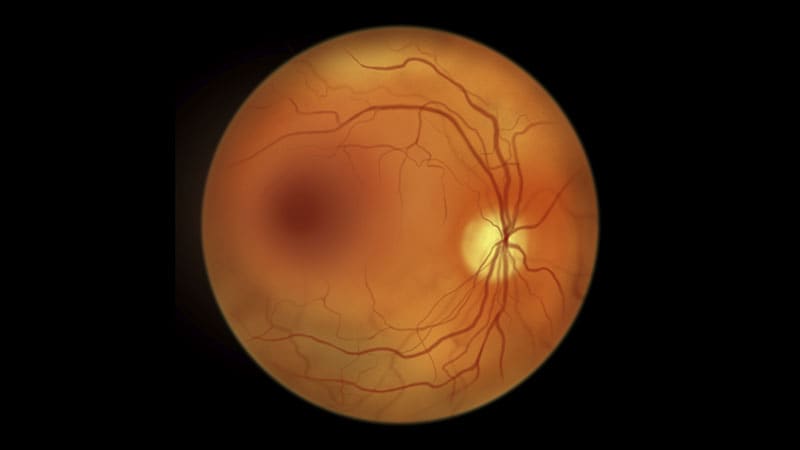
Prescribing of vaccines and drugs used in the treatment of glaucoma was correlated with lower deprivation.
“The dichotomy between drugs used in the treatment of diseases predominantly associated with lifestyle factors, which correlate with high deprivation, and those used as treatments for the non-lifestyle-associated diseases, which generally do not correlate with deprivation, is impossible to ignore,” the authors say.
Presenting the findings in Family Medicine & Community Health, they say the differing average prescription cost observed between different areas may represent development of newer and thus more expensive drugs for those diseases which are represented more equally across all areas.