Takeaway
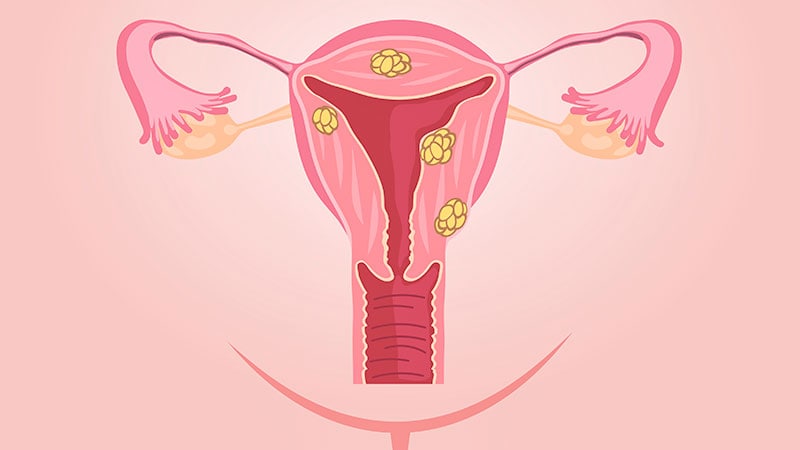
- In women with uterine fibroids (UF), elagolix plus add-back therapy significantly reduced heavy menstrual bleeding.
- Add-back therapy attenuated the decreases in bone mineral density (BMD) associated with elagolix alone.
Why this matter
- In a phase 2b study, elagolix (600 mg daily) with and without hormonal “add-back” therapy (to replace reduced levels of endogenous hormones) was effective in reducing menstrual bleeding and demonstrated favourable safety profile in women with UF.
Study design
- Study reported data from 2 identical phase 3 trials:
- Elaris UF-1: 412 women with UF were randomly assigned to receive elagolix plus add-back therapy (n=206), elagolix alone (n=104) or placebo (n=102).
- Elaris UF-2: 378 women with UF were randomly assigned to receive elagolix plus add-back therapy (n=189), elagolix alone (n=95) or placebo (n=94).
- Primary endpoint: heavy menstrual blood loss (MBL) <80 ml during the final month and a ≥50% reduction in MBL from baseline to the final month.
- Funding: AbbVie.
Key results
- Higher proportion of women in elagolix plus add-back therapy group (68.5% in UF-1 and 76.5% in UF-2) showed significant reduction in heavy MBL compared with those in the placebo group (8.7% in UF-1 and 10% in UF-2; P<.001 for both trials).
- Higher proportion of women in elagolix group achieved a significant reduction in heavy MBL (84.1% in UF-1 and 77% in UF-2 trial; P<.001).
- Hot flushes were frequently reported in a higher proportion of women who received elagolix plus add-back therapy (20.4% in UF-1 and 19.6% in UF-2) and elagolix alone (64.4% in UF-1 and 43% in UF-2) vs placebo (8.8% in UF-1 and 4% in UF-2).
- In UF-1 trial, metrorrhagia was significantly more common in elagolix plus add-back therapy vs placebo group (6.3% vs 0%).
- The mean percent reduction in BMD (except the femoral neck in UF-2) was diminished by add-back therapy.
References
References