These are the UK coronavirus stories you need to know about today.
Minute's Silence for Health Worker Deaths
Another 449 COVID-19 hospital deaths were reported today, taking the total to 16,509. The lower rise could be partly due to weekend reporting delays.
Of the 429 people who died in English hospitals, patients were aged between 40 and 101. Of those 15 aged between 49 and 92 had no known underlying health condition.
Commenting via the Science Media Centre, Prof Sir David Spiegelhalter, chair, Winton Centre for Risk and Evidence Communication, University of Cambridge, said: "NHS England now provide a very helpful graph showing the actual day people died, rather than when deaths were reported. This clearly shows we are in a steadily, but rather slowly, improving position since the peak of deaths 12 days ago on April 8th. But, judging from the experience in Italy, this could be a lengthy process."
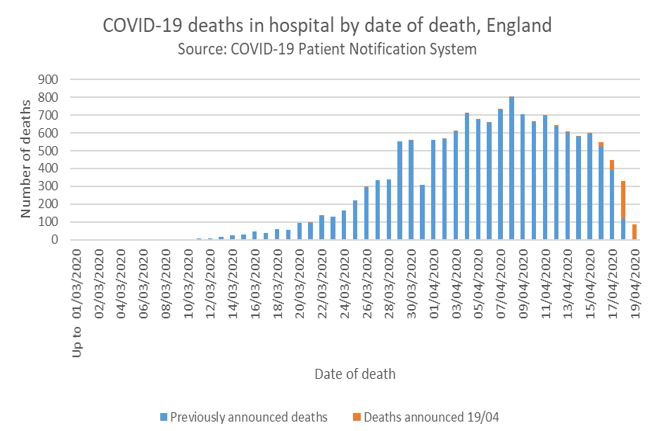
Graphic: NHS England
Was the large number of deaths in Liverpool due to 3000 Atletico Madrid fans travelling from a virus hotspot for the Champions League match with Liverpool FC? That was a question posed at today’s Downing Street briefing. The match on March 11th was allowed to go ahead in the weeks before the lockdown.
Deputy Chief Scientific Adviser Dame Angela McLean said: "I think it will be very interesting to see in the future when all the science is done, what relationship there is between the viruses that have circulated in Liverpool and the viruses that are circulated in Spain, that's certainly an interesting hypothesis."
Health unions are calling for a minute's silence for staff who have died due to COVID-19. The silence is planned for 11am on April 28th, which is International Workers’ Memorial Day.
There's already widespread support for Clap for Carers every Thursday evening. Royal College of Nursing General Secretary Donna Kinnair said: "We’ve become used to hearing a great roar on a Thursday night for key workers, but this respectful silence will be a poignant reminder of the risks they run to keep us safe.
"I hope the public gets behind this with the same affection they show when applauding our people."
Among recently announced NHS staff deaths was Margaret Tapley, 84, a nurse at Witney Community Hospital. She is believed to be the oldest NHS employee to have died after testing positive for COVID-19.
She was the "strongest woman I’ve ever met in my life," her granddaughter Hannah said on Facebook. "She was the most hard working, caring and perfect woman out there. Devoting her life to others and working for the NHS doing night shifts as a nurse at her age!"
The latest figure for the number of healthcare workers who’ve died in England from COVID-19 was given as 43 by the Department of Health. Today Nursing Notes said the figure through its tracking across the UK has passed 100.
In Memoriam: Healthcare Workers Who Have Died of COVID-19.
'The Issue Uppermost on People's Minds'
"Let me start by addressing the issue uppermost on people's minds: personal protective equipment or PPE," Chancellor Rishi Sunak said at the start of today's Downing Street briefing.
He again stressed that getting supplies was an "international challenge", adding: "We're working to resolve the Turkish shipment of PPE as soon as possible following some unexpected delays at the weekend."
"Today, we have unloaded a shipment of 140,000 gowns from Myanmar. And we are, of course, continuing to pursue every possible option for PPE procurement."
Mr Sunak was asked whether the Government was "ashamed" about PPE. He didn't give a direct answer.
PPE 'Adult Conversation'
Yesterday Dr Jenny Harries, deputy chief medical officer for England said: "I might say from my own professional perspective, we could perhaps have a more adult and more detailed conversation about PPE supplies."
Today Doctors’ Association UK Chair Dr Rinesh Parmar said: "Doctors have indeed been having both ‘adult and detailed conversations’ about the sheer lack of personal protective equipment for months, all of which have fallen on deaf ears.
"Since late February the Doctors’ Association UK and frontline doctors have been sounding the alarm about potential shortages, which have been met with misplaced reassurances that the UK has sufficient supplies."
Dr Parmar continued: "It signals a real disconnect between the Government and the daily experiences of frontline staff who have been reporting their PPE status in droves via our NHSppe.com. Doctors are risking their lives on the front line and deserve nothing less than the correct levels of PPE with no compromises whatsoever on their safety."
Dental Surgeons
Dental surgeons are the latest group to voice PPE concerns. A survey of nearly 200 dental surgeons by Royal College of Surgeons England (RCS) found 40% lack protective kit. One dental surgeon said PPE shortages have prevented urgent treatment centres from running. These are supposed to take patients while their own surgeries are closed.
In a statement Professor Michael Escudier, dean of the Faculty of Dental Surgery at the Royal College of Surgeons, said: "We welcomed NHS England’s recent guidance to dentists which was clear about the need for appropriate long-sleeved protection when we undertake procedures which create 'aerosol' sprays. But our survey shows access to PPE is already poor."
Plasma Trials
NHS Blood and Transplant (NHSBT) is asking for blood donations from people who have recovered from COVID-19 so it can be used in plasma therapy trials.
The BBC quotes a spokesperson: "If fully approved, the trials will investigate whether convalescent plasma transfusions could improve a COVID-19 patient's speed of recovery and chances of survival."
Trials and emergency use have already been approved in the US.
Testing Concerns
The Guardian spoke to an unnamed Public Health England (PHE) scientist who claimed its in-house tests, used since February, are performing worse than commercial kits. The paper cites a document saying “discordant results have been identified" with retesting needed for ambiguous results.
However, it quotes a PHE spokesperson saying: "There is no evidence to support that commercial tests are more accurate than the current PHE test. We believe the performance is comparable to currently available CE-marked assays [tests]."
A second Lighthouse 'mega-lab' for COVID-19 testing has opened at Alderley Park in Cheshire. National Testing Coordinator Professor John Newton said: "The Lighthouse Labs will be the biggest network of diagnostic testing facilities in British history. In unprecedented times, remarkable people across the country are achieving unprecedented things."
More News in Brief
- The Government has issued a 2000 word rebuttal of the Sunday Times article "38 days when Britain sleepwalked into disaster". Number 10 countered each allegation on a Department of Health blog with responses like "plainly untrue" and "ridiculous". The article said Boris Johnson "skipped" five emergency COBRA meetings and alleged complacency during January and February.
- Machine learning is being trialled to help predict future demand for ICU beds and ventilators for COVID-19 patients in England. The COVID 19 Capacity Planning and Analysis System (CPAS) is being trialled at four hospitals this week. NHS Digital Chief Medical Officer Professor Jonathan Benger said: "With the pressure being placed on intensive care by the current coronavirus pandemic it is essential to be able to predict demand for critical care beds, equipment and staff."
- Prince Philip praised health workers and scientists who are tackling coronavirus. In a rare public statement the 98-year-old said: "As we approach World Immunisation Week, I wanted to recognise the vital and urgent work being done by so many to tackle the pandemic; by those in the medical and scientific professions, at universities and research institutions, all united in working to protect us from COVID-19."