These are the UK coronavirus stories you need to know about today.
New Tiers
Areas of England have been allocated their new tiers ready for the end of national lockdown on December 2.
Birmingham and Manchester are in the highest Tier 3, London and Liverpool are in Tier 2.
Only three areas are in the lowest (medium) Tier 1: Cornwall, the Isle of Wight, and the Isles of Scilly.
Health secretary Matt Hancock told the Commons: "Current epidemiological evidence and clinical advice shows that we must make the tiers tougher than they were before to protect the NHS through the winter and avert another national lockdown."
Boris Johnson was out of self-isolation and back in the Commons for the announcement.
The Department of Health and Social Care said decisions on tiers are made by ministers based on public health recommendations. Factors include:
- Case detection rate, particularly in over 60s
- How quickly case rates are rising or falling
- Positivity in the general population
- Pressure on the NHS, including current capacity, admissions, general/acute/ICU bed occupancy, and staff absences
- Local context and exceptional circumstances, such as a local but contained outbreak
Areas may be moved up or down a tier based on new data with a review due on 16 December.
Areas in the highest Tier 3 are offered extra Test and Trace support with help from the armed forces for 6 weeks of lateral flow rapid community testing.
Positivity Rate 'Levelling Off'
The latest Office for National Statistics infection survey data show the positivity rate in England levelling off during recent weeks. Between 15 to 21 November 2020, ONS estimates 633,000 people had COVID-19, equating to around 1 in 85 people.
Increases in the positivity rate were only seen in secondary school children.
Ruth Studley from ONS commented: "At a national level in England, the overall number of infections appears to be levelling off." However, "There are considerable differences in rates across the country but the highest rates do remain in Yorkshire and the Humber, the North East, and the North West."
- Positivity rates in Scotland increased in the most recent week with 45,700 people having COVID-19, equating to 1 in 115 people.
- Positivity rates in Northern Ireland peaked around the middle of October. In the most recent week 12,700 people had COVID-19, equating to 1 in 145 people.
- Positivity rates in Wales peaked around the end of October. In the most recent week, 16,400 people had COVID-19, equating to 1 in 185 people.
Incidence data are not available this week due to problems at a laboratory.
Nowcast and Forecast
The latest nowcast and forecast for England from the MRC Biostatistics Unit, University of Cambridge, show:
- 41,200 new daily infections
- The number of daily deaths is likely to be between 205 and 317 on 5 December
- London, followed by the North West, continues to have the highest attack rate
PHE Data
Public Health England surveillance data show case rates have fallen across all age groups with the highest now in those aged 40 to 49.
The hospital admission rate for COVID-19 was 15.50 per 100,000 in the latest week compared to 16.88 per 100,000 the previous week.
Flu activity, including GP consultations and hospital admissions, remains low.
Flu vaccine uptake is higher in all groups except pregnant women compared to this time last year.
Daily Data
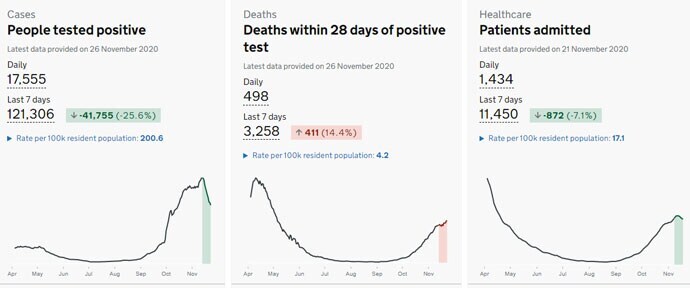
In today's daily data another 17,555 UK positive tests were reported and 498 deaths.
There are 16,341 COVID-19 patients in hospital and 1480 ventilator beds are in use.
Test and Trace
The latest performance data for England's Test and Trace programme, taking into account all contacts identified, show 39.7% weren’t reached.
Changes to the contact tracing process now mean that under-18s in a household no longer have to be contacted individually, as long as the parent or guardian in the household confirms they have completed their legal duty to inform their child to self-isolate.
System improvements saw an increase in the number of in-person test results being received the next day to 79.0% from 69.1% the previous week.
CPAP Success
Earlier use of CPAP for hospitalised COVID-19 patients saves up to 20% more lives, according to Lancaster University research published in BMJ Open Respiratory Research.
Dr Luigi Sedda from Lancaster said in a news release: "We show that continuous positive airway pressure (CPAP) in the first days of hospitalisation seems to save between 10% to 20% of patients. However it is important to underline that this was a pilot study with a small sample size, although comforting evidence is starting to emerge elsewhere."
The findings are based on patients admitted to the Royal Albert Edward Infirmary in Wigan.
Consultant respiratory physician Dr Abdul Ashish said: "As CPAP is readily available and can be used in a ward setting, we have demonstrated that, when used early, it can be a very effective way of treating severe COVID-19 pneumonia."
Emergency Department Data
Pandemic Respiratory Infection Emergency System Triage (PRIEST) data has been published in PLOS ONE on 22,445 people from 70 UK hospitals with suspected COVID-19 between March and May.
- On average, patients were 58.4 years old, 50.4% female, and 84.75% White.
- Adults admitted with confirmed COVID-19 were more than twice as likely to die or receive organ support than adults who did not have COVID-19.
- Adults had worse outcomes than children.
- Men were more likely to be admitted to the hospital than women (72.9% vs 61.4%), more likely to require organ support (12.2% vs 7.7%), and were more likely to die (18.7% vs 13.3%).
- There were ethnicity differences with Black and Asian patients more likely than White to require organ support (15.9%, 14.3%, 8.9%) and were more likely to have a positive COVID-19 test (40.8%, 42.1%, 30.0%).
The authors, led by the University of Sheffield, said: "Our findings show that people attending emergency departments with suspected COVID-19 were seriously ill, suggesting that policies aimed at diverting less serious cases away from hospitals were successful. We also showed that admission with COVID-19 carries a much higher risk of death or need for life-saving treatment than admission with similar conditions."
See more global coronavirus updates in Medscape’s Coronavirus Resource Centre.





