Takeaway
- 7 days of antibiotic therapy is noninferior to a 14-day course in haemodynamically stable patients hospitalised for gram-negative bacteraemia.
Why this matters
- A shorter course limits antibiotic exposure and allows earlier return to baseline functional capacity.
Key results
- 604 patients (306 short-, 298 long-duration arms).
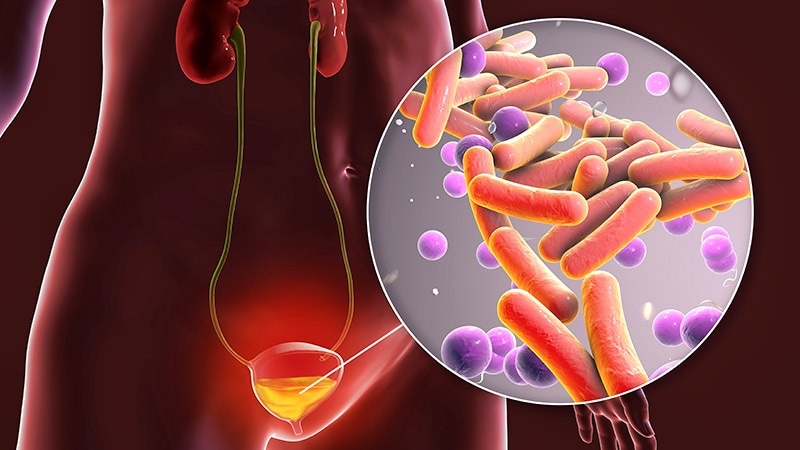
- Primary bacteraemia source: urinary tract (68%), main pathogen: Enterobacteriaceae (89.9%).
- Primary 90-day endpoint was met by 45.8% (140/306) and 48.3% (144/298) of patients receiving 7- and 14-day antibiotics, respectively.
- Primary endpoint defined as mortality, clinical failure, readmission, or extended hospitalisation: risk difference (RD), −2.6% (95% CI, −10.5% to 5.3%).
- Stratified analysis: RD, −2.7% (95% CI, −10.7% to 5.2%).
- Per-protocol analysis: endpoint met by 45.7% (128/280) and 47.8% (132/276) of patients receiving 7- and 14-day antibiotics, respectively (RD, −2.1%; 95% CI, −10.4% to 6.2%).
- No mortality differences observed at 14 or 28 days; no difference in complications.
- Time to return to baseline activity ≤90 days was significantly shorter with 7-day course (median, 2 [interquartile range (IQR), 0-8.3] weeks vs 3 [IQR, 1-12] weeks).
Study design
- Randomised, open-label, noninferiority study analysing 7- vs 14-day antibiotic courses in hospitalised Italian, Israeli patients with gram-negative bacteraemia.
- Funding: None disclosed.
Limitations
- Findings limited to gram-negative nonfermenters.
- Inability to demonstrate influence on resistance.
- Potential to shorten hospital length of stay not demonstrated.
References
References